Topics
- Article
- Health & Wellness
What is the Health Operating System?

The Holy Grail of Health
Every society has chased the same dream: to live longer and to live better. Egyptian pharaohs poured fortunes into tombs and preservation rituals, hoping to carry their bodies into eternity. Qin Shi Huang, China’s first emperor, sent expeditions for an elixir of immortality. European monarchs bankrolled alchemists in search of the philosopher’s stone. Ponce de León crossed oceans in pursuit of a fountain of youth. Indian and Persian rulers commissioned elixirs, tonics, and yogic practices to stave off decline. And in recent decades, billions have been poured into longevity biotech and cryonics. These are modern echoes of the same quest.
For most of history, this pursuit was fantasy. Lifespan crept upward, but healthspan, the years we spend truly well, lagged behind. Humanity learned to extend survival, but not vitality. And despite extraordinary advances in biology and medicine, the system of health in most modern nations has not closed that gap.
The uncomfortable reality is that the system underlying modern medicine was never designed around people. It was built around institutions: hospitals, regulators, insurers, pharmaceutical companies, billing codes. The system is episodic, reactive, and transactional.
Indeed this system is not designed to keep you healthy. It is designed to manage your illness. That is a noble mission in moments of crisis: a cancer patient guided through remission, a heart attack survivor stabilized by an emergency team, an ALS patient kept alive on a feeding tube. These are miracles. But they are miracles that exist in the paradigm of reactive care, not in the pursuit of vitality. Now, a new kind of actor is emerging. Across industries, AI tools already book travel, trade stocks, manage supply chains, and even write software. At their core, these agents perceive environments, make decisions, and take actions autonomously to achieve goals.
In health, similar technology will perceive your biology as its environment. It will track how sleep fuels recovery, how recovery shapes performance, how performance generates stress, and how stress cycles back into sleep. But the technology won’t stop at observation: it will intervene, nudging behaviors, adapting routines, and even initiating care when risk rises. In this way, new technology will transform hidden feedback loops into an intelligent, always-on system for extending vitality and preventing crisis.
This is the threshold we now face: the AI epoch of health. Foundation models, trained on massive unstructured data, reasoning across modalities, personalizing to individuals, and predicting trajectories, make possible what no pharaoh, emperor, or alchemist could have imagined: a true Health Operating System.
The Health OS brings hidden biological loops to the surface, revealing them in real time and intervening to reduce risk and deliver care. Its core mission will be to understand, predict, and direct these cycles. This will usher in changes that will transform health as we know it.
Why the Old System Cannot Survive
What most call “healthcare innovation” today is a thin digital skin stretched over a broken operating system. Electronic health records, telemedicine portals, automated claims processing. These are not paradigm shifts. They are clunky upgrades to a teetering system.
The United States health care system is the perfect example of a system in crisis. Healthcare costs are surging to unprecedented levels, but the outcomes they purport to deliver are falling short and even backsliding. U.S. national health spending exploded from roughly $1.4 trillion in 2000 to $4.5 trillion in 2022, tripling in just two decades, and now consumes about 17 percent of the U.S. economy. Americans now spend more on healthcare expenditures than groceries or housing.
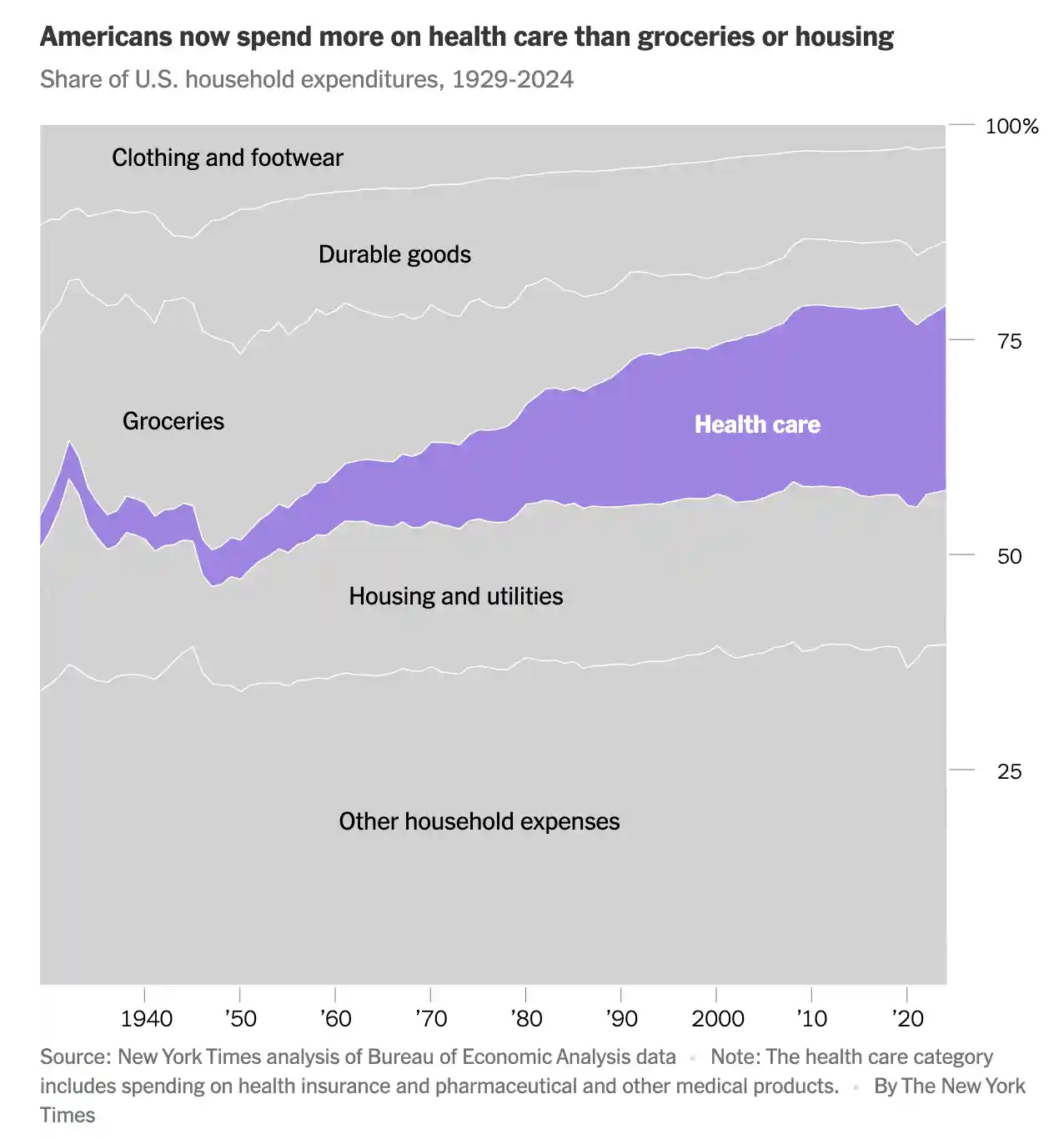
Credit: The New York Times (2025)
Yet despite being the only high-income country without universal coverage, and spending nearly twice as much per capita as peer nations, the United States trails them across crucial health metrics, exhibiting the lowest life expectancy, highest rates of infant and maternal mortality, and some of the highest rates of avoidable mortality. The Commonwealth Fund estimates that administrative expenditures alone contribute to about 15 percent of the country’s excess per capita health spending compared with peer countries. Meanwhile, chronic diseases are on the rise. A 2025 study found that 76.4% of U.S. adults report one or more chronic conditions. In short: the U.S. is hemorrhaging money, yet failing to deliver healthier lives.
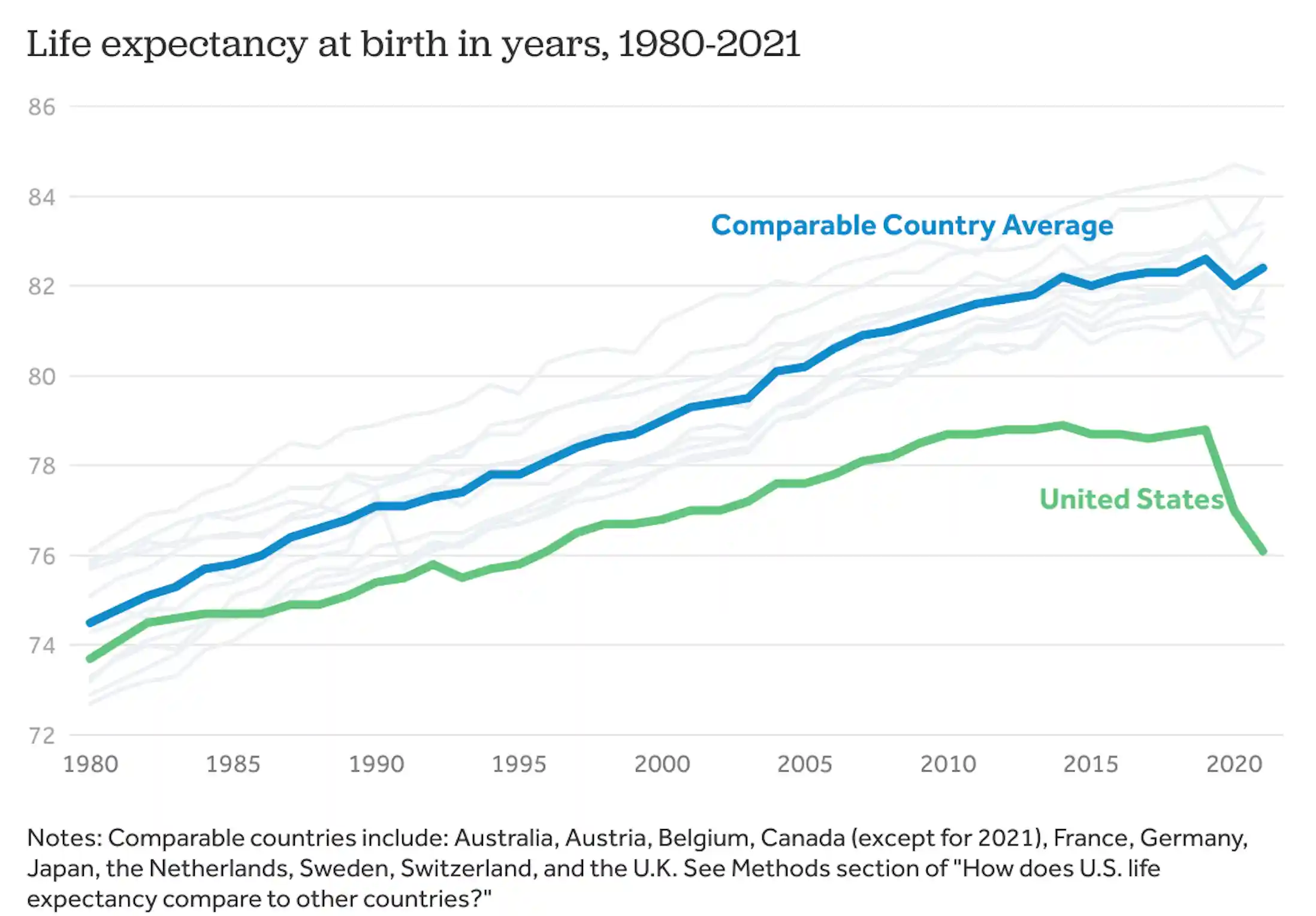
Source: Peterson-KFF Health System Tracker
Despite the excitement around new innovation, the incumbent players are trapped by structural flaws they cannot escape:
- Incentives are misaligned. Insurers make money when risk is mispriced, not when people get healthier. Hospitals profit when beds are full, not when they are empty. Pharma thrives on chronic disease management, not prevention.
- Data is episodic. A “medical record” is a handful of test results and physician notes spread across decades. It is not a living picture of your body.
- Technology debt is crippling. Hospital IT systems are decades old and cannot integrate multimodal AI that requires petabytes of streaming data.
- Culture resists change. Incumbents are structured to protect revenue streams, not to build radically new systems.
- The system is too reliant on humans who are inherently fallible. Broken systems and feedback loops also pose dangerous risks. Within the United States, at least 1.5 million medication-related errors occur each year. These mistakes may largely be unintentional, but their consequences are severe.
Could the established players build a new system themselves? In theory, yes. In practice, no. They lack the data, the aligned incentives, and the technical agility. By the time they try, the new Health OS will already be dominant. This story is familiar. Retailers couldn’t out-Amazon Amazon. Taxi companies couldn’t out-Uber Uber. Legacy media couldn’t out-Netflix Netflix. Healthcare incumbents will not out-innovate platforms that are born AI-first.
Transforming How We Experience Care
The defining difference of the new Health OS is that it flips healthcare on its head. Today, the health infrastructure delivers services to individuals; tomorrow, individuals are the infrastructure. Care will no longer be episodic and institution-centric, but literally centered and personalized within each person and driven by the continuous biometric signals their own body produces.
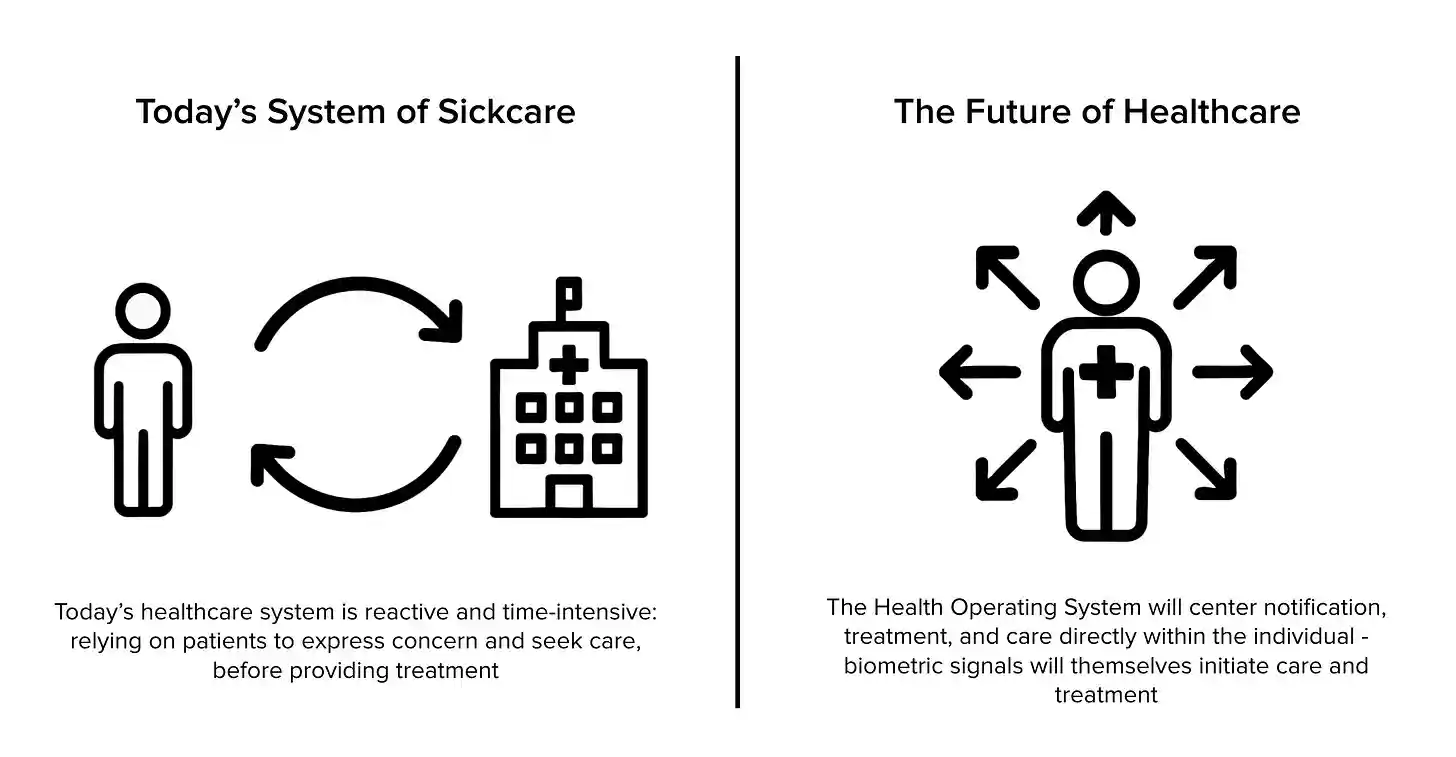
That is the fundamental shift: the individual becomes the hub of the system, not a passive node within it. Healthcare moves from reacting to crises to preempting them, with new technology transforming the body’s signals into real-time intelligence that powers care. This technology will take many forms, interpreting biometric data, reasoning about health trajectories, and then taking autonomous action to support an individual.
For individuals, the shift will be nothing short of profound. What once required waiting for symptoms, booking an appointment, and receiving episodic treatment will be replaced by constant partnership with AI-enabled agents working silently in the background of daily life. Care will feel less like a transaction with the healthcare system and more like an ongoing conversation with your own body, mediated by technology that never sleeps. The differences will include:
No more annual check-ups.
The concept of a yearly exam will vanish. Instead, your body will be continuously monitored across hundreds of dimensions - sleep, recovery, stress, blood pressure, hormones, cognition, diet, feelings- creating a living health record that updates in real time. These are the earliest building blocks of a true Health OS. Indeed, the very nature of a “health record” will be replaced by dynamic reporting that’s always changing and reassessing risks. Small deviations will be caught early, eliminating the need to compress an entire year of medical assessment into a single visit. Wearables like WHOOP have already pioneered this shift, building longitudinal health records across sleep, recovery, and strain. To be clear, doctors won’t summarily disappear, but the profession will change. Dr. Eric Topol, the American cardiologist, has put it well: AI will not replace physicians, but physicians using AI will soon replace those not using it. And people will have access to medical insights even without these physicians.
Intervening before crisis.
The new system will fundamentally change how we handle crisis in healthcare. Consider a stroke. In today’s “sick care” system, nothing happens until the patient recognizes symptoms (numbness, slurred speech, confusion) and initiates contact by calling 911 or seeking emergency care. Only then does the system begin: diagnosis, treatment, monitoring, and - hopefully - recovery. By contrast, the future Health OS will detect the earliest physiological precursors (rising blood pressure, declining heart rate variability, atrial fibrillation) long before visible symptoms appear. Emergency services could be alerted automatically, with care mobilized before the patient even realizes they are at risk. The hospital staff will know exactly when the patient is arriving and why - no need for triage. This matters because stroke outcomes are measured in minutes: Yale researchers found that more than half of patients arrive at the hospital outside the critical two-hour window for effective treatment, and each 10-minute delay can cost weeks of healthy life. The Health OS will collapse those delays, converting the slowest, most failure-prone link in the chain - the patient’s recognition and response - into an instant, automated trigger for care. The result is not just faster treatment but also the possibility of preventing catastrophic brain damage altogether.
More precise recovery.
After an injury or surgery, guessing when you can safely return to work, exercise, or play will no longer be necessary. The system will analyze healing signals and patterns unique to your physiology and tell you, with precision, when your body is ready. This prevents setbacks and accelerates rehabilitation.
Personalized prescriptions.
Instead of one-size-fits-all medications, the Health OS will formulate treatments designed for your individual biology. Foundation models integrating genomic data, biomarkers, and lifestyle context will enable dosing, drug selection, and even compound creation that reflect your physiology, not a population average. Every prescription will feel as though it was made for you, because it was. This will mitigate the immense risk attributable to adverse drug events and deadly polypharmacy mistakes.
Everyday direction, not abstract advice.
Instead of generic reminders like “eat better” or “reduce stress,” the Health OS will give you precise, actionable nudges at the exact moment they matter. It might tell you to skip an espresso because your cortisol is spiking, or to step outside for ten minutes of sunlight to rebalance your circadian rhythm. If biometric sensors see changes in your body temperature variability, heart rate, and blood pressure, the Health OS may trigger an urgent nudge: “Go to the ER now. Your biomarkers indicate possible infection escalation.” Each intervention is individualized, reflecting your unique biology and context, not a population average.
Agents as advocates.
Intelligent agents will serve as round-the-clock advocates, translating massive streams of health data into clear next steps. They will escalate urgent issues to clinicians, automate routine monitoring, prescribe personalized interventions, and help you make informed choices. Instead of relying on a physician’s occasional visit, you’ll be supported by a system that knows your health history better than any single doctor ever could.
This is what it means to live inside this new Health OS: health that is always-on, preventive rather than reactive, personalized instead of generic.
The Technical Advances That Make This Moment Possible
For decades, digital health promised transformation but delivered only fragments. What sets this moment apart is that the enabling technologies have finally arrived.
I experienced this fragmentation firsthand while building WHOOP. For years, digital health tools could track isolated metrics, like steps, calories, or workouts. But they rarely connected the dots in a meaningful way. WHOOP set out to change that by measuring sleep, recovery, and strain as an integrated system, creating one of the first continuous health records of its kind. That experience made clear both how powerful connected data can be, and how much more is possible when new technologies converge.
And yet this is just the beginning. The convergence of multiple breakthroughs has led to possibilities that most could not have imagined years ago. Each is powerful on its own. Together, they are an unstoppable force for improved health outcomes.
1. Architectures that leverage data and compute efficiently.
Advances in model design, from transformers to multimodal embeddings to self-supervised learning, have unlocked new ways of making sense of massive, messy health data. These systems can align signals across physiology, behavior, and environment, drawing meaning from billions of unlabeled data points. When coupled with modern compute, this shift makes it possible to process huge histories of biometrics, uncover subtle patterns, and generate forecasts that were unimaginable just a few years ago. This allows the Health OS to uncover deeper insights into sleep, recovery, and disease progression. This also allows the ability to personalize guidance at scale.
2. Advances in reasoning, explainability, and memory.
Traditional health analysis has always been static: one lab result, one snapshot. New reasoning capabilities allow AI to understand trajectories, rhythms, and causal links across time. Just as important, advances in explainability mean predictions are no longer opaque. Members can see not just what is changing, but why, with attribution across behaviors, biomarkers, and sleep patterns. And because these systems remember, integrating years of health history into every assessment, guidance becomes richer and more trustworthy over time. When combined, reasoning, explainability, and memory transform AI from a black box into a trusted collaborator. They turn raw data into clear roadmaps for action.
3. Intelligence at the edge.
Health decisions often cannot wait for cloud processing. With edge inference, models can now be “always on,” running directly on wearables and sensors. That means guidance without latency: a timely nudge to de-stress, an early warning before a heart attack even when you don’t have WiFi, instant health feedback. On-device AI turns the Health OS into an active companion, always present and always responsive.
These three advances combine to create a backbone for the Health OS that’s both powerful and practical. In concert, they unlock proactive, personalized, and trustworthy health guidance at scale. This is something the world has never had until now.
The Societal Consequences
The consequences of this new Health OS cannot be overstated. This is not just another wave of digital health. It is a fundamental rewiring of society’s most human pursuit: the quest for vitality, performance, and longevity. Entire industries will be reordered. Cultural norms will be reshaped. Governments will face existential choices.
It is impossible to know exactly how this will play out or who will be most impacted, but these trends are likely to lead to the following outcomes:
1. Insurance will be more dynamic than ever before.
The opaque pricing models of health insurance will collapse. When risk can be assessed in real time - with dynamic, transparent scoring based on continuous physiology - the business model of insurance changes. Those who adopt the Health OS will enjoy lower premiums, creating pressure for universal adoption. Insurers that fail to adapt will find themselves disintermediated.
2. The pharmaceutical industry’s incentives will shift to precision.
Pharma’s current model thrives on managing chronic conditions rather than preventing them. The Health OS threatens this model. If hypertension can be flagged and reversed years before diagnosis, the market for blood pressure medications shrinks. On the other hand, pharma that embraces the OS can thrive by creating precision therapies that integrate with real-time monitoring. Drug development itself may become faster, as population-scale data accelerates discovery of biomarkers and treatment effects. Pharma does not need to lose in this system. But they do need to evolve.
3. Special Interests will present the biggest obstacle.
The policy implications are profound. Health costs are among the largest budgetary burdens for every advanced nation. That also means that there are many special interests that benefit from the current system. A Health OS that lowers costs while extending lifespan is a once-in-history opportunity. Governments will have to decide whether to defend incumbents or accelerate adoption. Some may subsidize the OS to improve national competitiveness. Others may resist, only to watch their populations and economies fall behind. This will become a matter of national security.
4. Healthspan accessible to all.
The cultural consequences may be even greater. Health will be accessible to everyone at all times. The same insights once reserved for elite athletes or the wealthiest citizens will be available to everyone. Over time, the very definition of health will shift from absence of disease to optimization of human potential. This is something I witnessed building WHOOP: our technology initially calibrated for Michael Phelps and LeBron James became relevant for and used by millions of people.
Today, access to the best smartphone has little to do with one’s wealth. In the future, the same ubiquity and accessibility will apply to health. When the Health OS can be delivered through a wearable paired with advanced AI technology, then billions of people who never had access to modern healthcare can leapfrog into continuous, improved health. Just as mobile phones leapfrogged landlines in the developing world, the Health OS can leapfrog clinics and hospitals. This has the potential to narrow global health disparities on a historic scale.
5. We will live longer than ever before.
I am convinced that there are people on this planet today that will live healthy lives until 150. It may sound radical to suggest that there are people alive today who will live that long, let alone live that long well. Yet when you consider the trajectory of technology, that estimate may be even too conservative. The Health OS represents the most significant shift in human longevity since the discovery of antibiotics. By continuously sensing physiology, predicting risks before they appear, and delivering personalized interventions in real time, it compresses morbidity and extends vitality in ways medicine has never before achieved.
The Result: More Healthy Years
Many companies will pursue building aspects of this Health OS. Success will belong to the few that can fuse massive, continuous health data with cutting-edge AI and deliver daily, trusted engagement that becomes inseparable from people’s lives. It is easier to envision the Health OS than actually build it, but there is no question this will exist in just a few years time.
At WHOOP, we believe we have the ingredients and the team to tackle this opportunity. WHOOP has spent over a decade building the world’s most robust longitudinal dataset on human performance, recovery, and behavior. We have prioritized three critical factors: the most robust 24/7 health data, daily engagement with our members, and an advanced AI layer that sits within the product. We believe there is no better foundation on which the Health OS can be built.
Ultimately, this is bigger than any one company. It is about completing humanity’s oldest pursuit: the quest for vitality. Health is not your last doctor’s visit, not a billing code, not a prescription written after symptoms appear. Health is a continuous state, dynamic, adaptive, and improvable, and for the first time in history we have the technology to measure it, model it, and improve it at scale. The dawn of the new Health OS represents not just another tool, but a new epoch in how humanity approaches life itself.
The data makes the stakes clear. A 2025 study found that while lifespan has steadily increased, healthspan has lagged behind, leaving millions to endure decades of poor health, disability, or chronic illness. A slowdown in aging that adds just one healthy year to human life is valued at $38 trillion to society, while a ten-year gain is valued at $367 trillion. The social return on even a single healthy year is immense.
And yet beyond the numbers, the truth is more significant. One more year of health means one more holiday with family, one more birthday celebrated, one more chance to live fully. For an individual, that year is priceless. For humanity, multiplied by billions, it is the Holy Grail.
For centuries, pharaohs, emperors, and explorers sought this prize in vain. Today, it is within reach. The next operating system for humanity will not just make us more connected or more productive. It will extend our healthspan. The dawn of the new Health OS is not about powering machines. It is about powering life itself.
–Will Ahmed