Topics
- Article
- App & Features
- Women’s Performance
Sleep Planner Update: Incorporating Menstrual Cycle Phase for Increased Accuracy
We explain the physiological changes caused by the menstrual cycle, the effect hormonal birth control has on it, and how the WHOOP Sleep Planner now takes all of this into account.
The only part of the menstrual cycle that seems to get any attention is the menstruation part. Commonly referred to as “the period” or more shyly as “that time of the month,” this is just one small piece of a beautifully intricate cycle of hormones that affects much more than our chances of getting pregnant, but also how we sleep, recover and respond to training. If you’re not afraid of a little blood, I’m about to take you through the physiology of the menstrual cycle, how hormonal birth control changes that physiology, and how WHOOP is accounting for those physiological changes in a new update to the Sleep Planner.
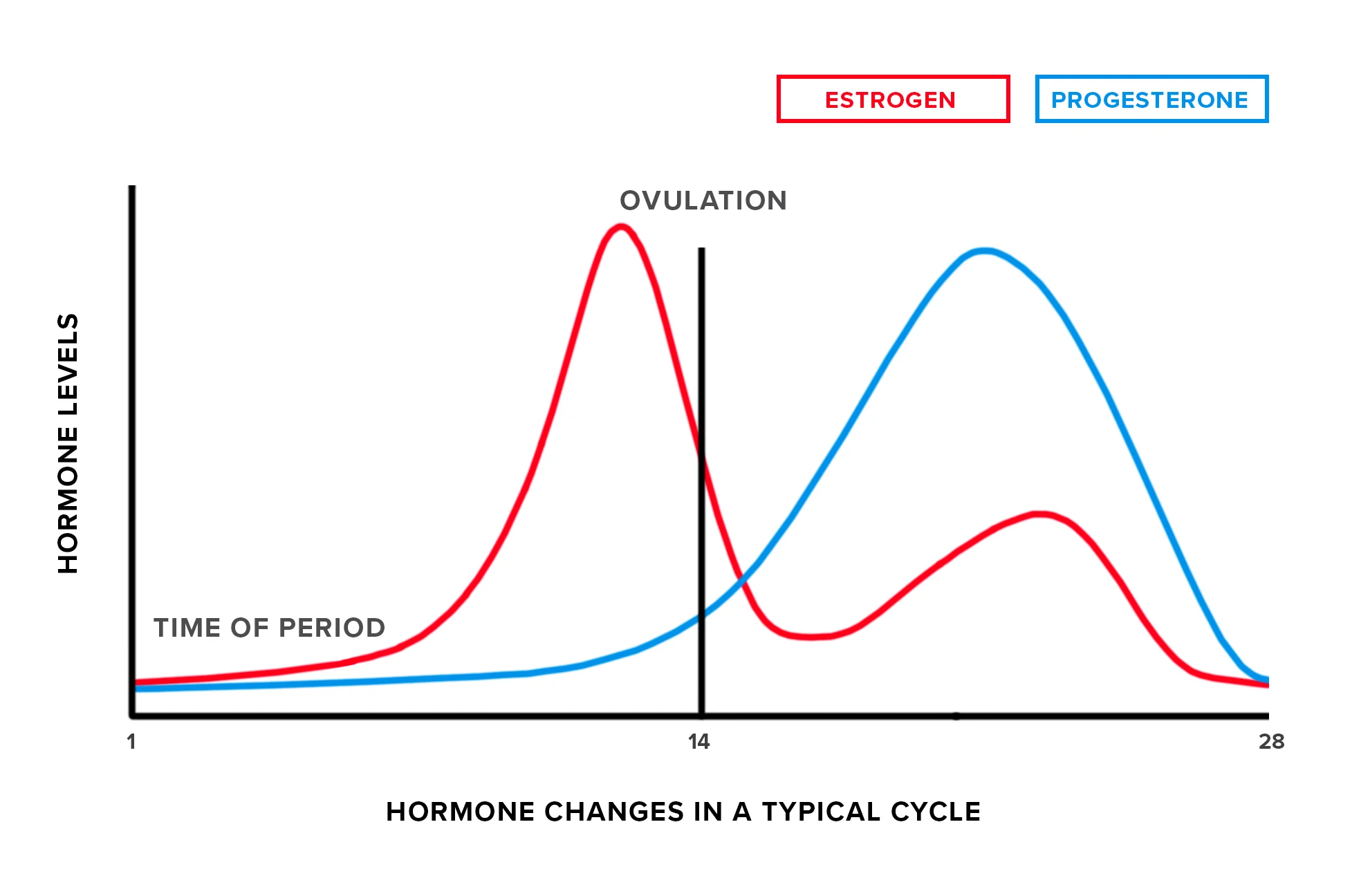
Menstrual Cycle Phases
At a high level, the menstrual cycle can be broken down into two phases. The first phase is called the follicular phase, which starts on the first day of menstruation (bleeding) and ends 11-27 days later with ovulation (releasing an egg). The luteal phase completes the cycle, running from ovulation to just before menstruation begins. These cycles continue one after the other as long as they aren’t interrupted by pregnancy, menopause, or health issues, but we’re not going to talk about those things here. Those of us who menstruate are born with all the eggs we will ever produce already made, but in a half-baked state. The follicular phase is defined by the release of hormones that tell our ovaries (the egg storage organs) to produce sacs called follicles containing those immature eggs. Although we get a few follicles each menstrual cycle, typically around 20, only one (or occasionally more, as in the case of twins or higher-order multiples) will win out and turn into a mature egg released to the uterus in search of sperm. While this is happening with our eggs, our uterus is simultaneously preparing for the egg’s arrival by thickening its lining and enriching it with life-sustaining nutrients. You can think of the uterus as the perpetual optimist, preparing for each egg’s arrival as if it will be fertilized and hang around for 40 weeks transforming into a full-on human. Increases in Progesterone and Estrogen The release of the egg into the uterus is called ovulation. This event marks the end of the follicular phase and the start of the 11-17 day luteal phase. Ovulation is also the time in the cycle when you can get pregnant. In hopes of a fertilized egg implanting, the luteal phase brings with it increases in two key hormones, progesterone and estrogen. Even though our uterus did so much great work to prepare for the egg’s long term stay, if it isn’t fertilized within about a day of release, it will die. When the uterus gets the hint that it will not be hosting a fetus this month, the ovarian hormones drop. This causes the changes to the uterine lining that were made to sustain the pregnancy to reverse, ultimately resulting in your period (ie: the start of the next follicular phase) and the cycle beginning again.
Effect of Hormonal Birth Control
Many people who menstruate choose to alter these hormonal cycles using hormonal birth control (HBC). People choose to use HBC to avoid pregnancy or just to avoid the unwanted symptoms the cycling hormones can have, such as painful cramps and acne breakouts. Not all birth control is hormonal. Other options prevent pregnancy by creating a physical barrier between the sperm and egg (like a condom), or by killing the egg (like a copper IUD) or sperm (like a spermicide) so they can’t successfully meet and fertilize. HBCs come in many forms, from the popular pills, to vaginal rings, implants, injections, and IUDs. These birth control forms are all just different delivery devices of the two primary hormones mentioned above, progesterone and estrogen. These hormones are either delivered together or just progesterone is used. Either way, they work by preventing ovulation (egg release), meaning that even if sperm show up, there is nothing to fertilize. Here’s the thing though--if you are on HBC, even if you get a period the hormones in your birth control are dominating over your natural cycle. So while pre-HBC you might have had a cycle that looks like this the graphic pictured above, you now have a cycle that looks like this:
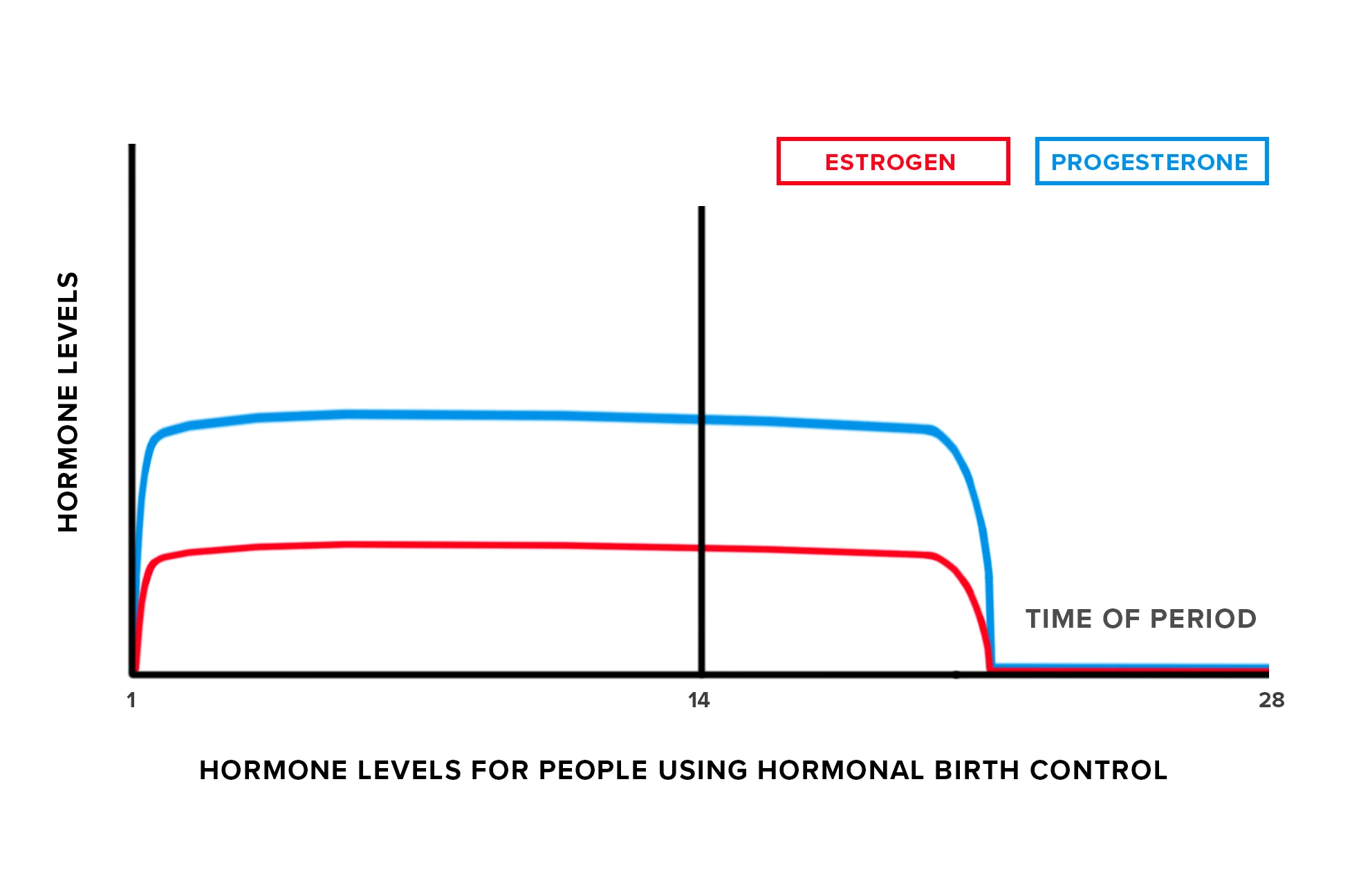
The now evened-out hormones prevent the symptoms related to fluctuations, but also mean that what we’re about to dig into in the remainder of this article will not apply to you because you don’t have hormonally distinct follicular and luteal phases.
Menstrual Cycle and Sleep
Although the menstrual cycle is mostly about reproduction, its effects span all our systems including our circadian rhythm (biological clock best known for its role in regulating sleep and wake timing) and sleep architecture (fancy term for the distribution of sleep stages during a sleep). The premenstrual week - the end of the luteal phase right before menstruation begins - is known to be associated with relatively lower quality sleep and more time spent awake than during the rest of the cycle. Because sleep efficiency will vary by menstrual cycle phase, people who menstruate can plan to allow for more time in bed during the late luteal phase to offset the reduced efficiency. For example, if you typically get 7.5 hours of sleep in an 8-hour sleep opportunity, you may want to give yourself an 8.25 hour opportunity to get that same 7.5 hours of sleep you need to feel your best. The exact amount of reduced sleep efficiency will vary from person to person depending on how sensitive you are to these hormonal changes, so we’ve updated the WHOOP Sleep Planner to learn your individualized response to each menstrual cycle phase and to incorporate this into a more personalized recommendation. To take advantage of this new feature, you’ll need to track your menstrual cycle using the WHOOP Journal. You can also now log each of the following in the journal: Nursing an infant, hot flashes during sleep, menstrual cramps, bloating and ovulating.
How to Enable Menstrual Cycle Sleep Planning in the WHOOP App
1. Make sure you have the latest version of our app installed, then enter the WHOOP Journal from the overview screen. 2. Click the pencil icon to edit your journal. 3. Click the settings icon in the top right corner to customize your journal. 4. Scroll to the right to the “Reproductive Health” tab. 5. Click the plus sign to enable the menstruating toggle or if you already have the toggle enabled, click the “On birth control?” box below the menstruating line item.
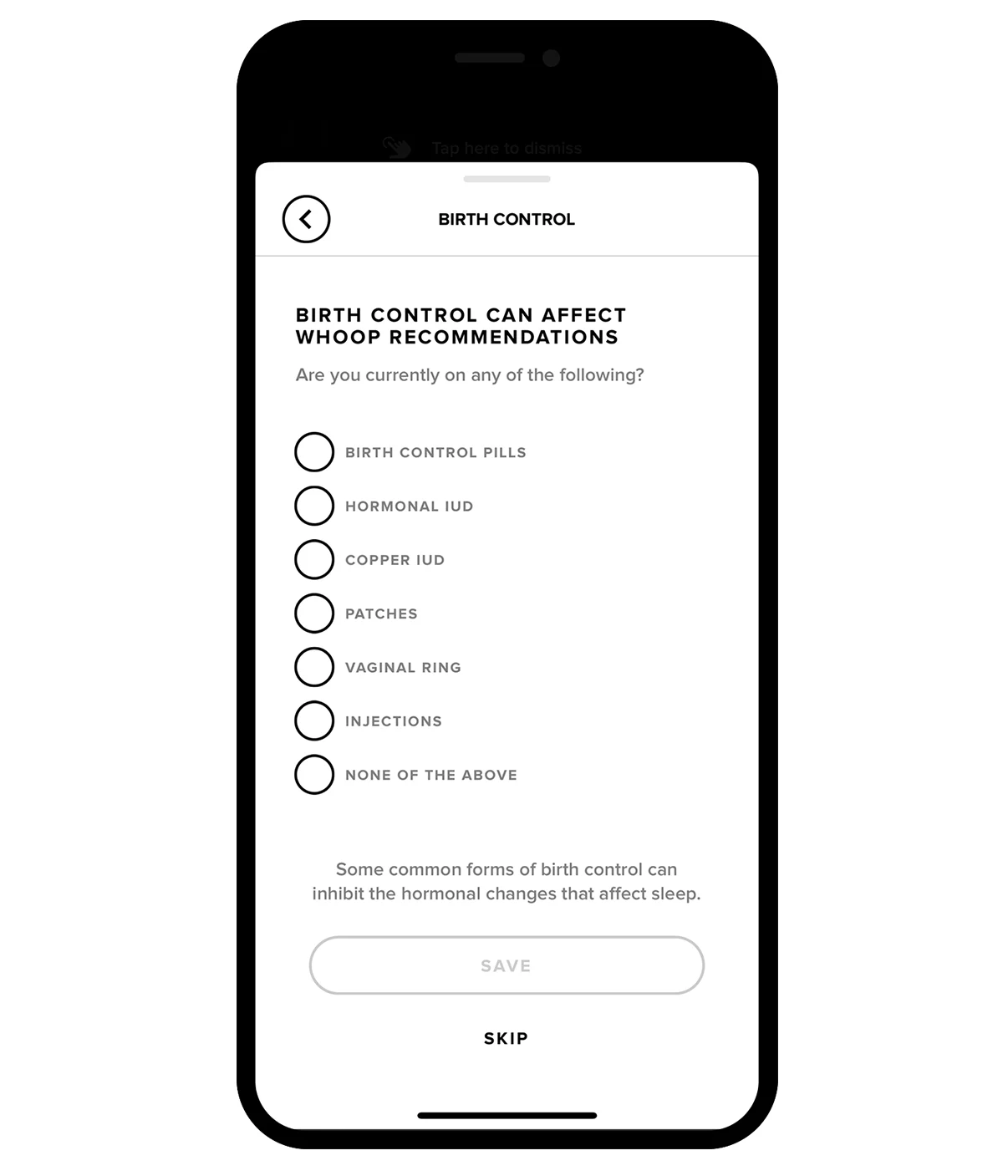
6. Answer the question related to birth control (Note: only users who are on a Copper IUD or “None of the above” are eligible to receive this feature). 7. Tap save. 8. Read the message indicating you must continue to use the Journal daily to track your cycle and tap “Got it.” 9. We will then send you an in-app pop up message when the feature has been enabled for you! This may be within 24-48 hours if you have already been tracking your menstrual cycle in the WHOOP Journal. If you are new to this, there is a one-cycle calibration period (roughly one month) before your Sleep Planner recommendations will switch over to menstrual-cycle based coaching.